The HIPAA Minimum Necessary Standard Explained

Written by
John MartinezLast updated on:
June 26, 2025Reading time:
Contents
Built for Security. Loved by Devs.
- Free Trial — No Credit Card Needed
- Full Access to All Features
- Trusted by the Fortune 100, early startups, and everyone in between
This article gives you a broad look at the Health Insurance Portability and Accountability Act (HIPAA) minimum necessary standard. You’ll learn about its requirements and exceptions, as well as how to implement it. By the end of the article, you’ll know how the HIPAA minimum necessary standard applies to you and how to develop your own internal processes for compliance.
What Is the HIPAA Minimum Necessary Standard?
The HIPAA minimum necessary standard applies to companies that comply with the HIPAA privacy rule. It compels organizations to take reasonable actions to limit the sharing of protected health information (PHI) as part of record requests. What is “HIPAA’s minimum necessary rule?” It’s not a rule but a standard of agreed practices.
But what does the HIPAA minimum necessary standard for PHI mean? The minimum necessary standard of the HIPAA privacy rule encourages covered entities to decide which information to share and the reasonable steps to take to protect PHI. What does the privacy rule require? It’s the broader rule about who’s required to protect patient records and appropriate uses of private data.
The PHI minimum necessary rule applies to people in the practice and to each data category. These practitioners adhere to the minimum necessary HIPAA rule by following policies about which staff members can access patient files and the details they can access within a patient’s file.
First, organizations limit access to records by job role or responsibility. For instance, privacy officers restrict patient file access to the health care professionals who treat patients, while excluding access from other providers within the medical practice. Second, they meet the standard by limiting access to sensitive data, like birthdates or treatment notes, in patient files.
HIPAA Minimum Necessary Standard Examples
HIPAA includes the minimum necessary standard. It essentially refers to when providers and third parties can have more than the least amount of essential data to do their jobs. What the minimum necessary rule means depends on a couple of factors. The most crucial aspect is having the least amount of information in as few hands as possible, that is, furnishing only the crucial details required to provide a service.
Keep in mind the following examples of how you can use the standard to avoid penalties:
- IT teams must check for cybersecurity breaches without viewing patient records by opening and accessing them.
- Administrative teams must give treatment teams patient records that exclude social security numbers, billing information, and other sensitive data unrelated to treatment.
- Billing teams must be able to access the names of the tests physicians performed but not the results.
- Insurance companies and law enforcement must not have access to full patient histories. When responding to a request, an organization must provide only the records that are suitable for assessing a current situation.
- Third parties that investigate a crime must receive relevant injury records, not a patient’s entire medical history unrelated to the injury under investigation.
- Practitioners must never mention a medical diagnosis in unprotected physical space in earshot of unauthorized personnel. They must shield verbal and even paper-based records from outside parties.
For tasks related to medical records, employees should have access only to the PHI needed to complete the task. Care providers are limited in the medical information they can access for their patients: if it’s unrelated to the treatment at hand, it’s off-limits.
How Does the Minimum Necessary Standard Work?
The U.S. Department of Health and Human Services offers guidance on the minimum necessary requirement of HIPAA for individuals and organizations. Individuals can find information about their rights and how to file a complaint. Meanwhile, professionals can access summaries of every rule and enforcement information. They can also learn about obligations like breach notification.
Which organizations are affected
If your organization is just starting to meet the minimum necessary rule in HIPAA regulations, first examine your status and determine if you’re a covered entity held to the standard. It includes the following covered entities:
- Clearinghouses
- Clinics
- Chiropractors
- Dentists
- Doctors
- Health plans
- Nursing homes
- Pharmacies
- Providers that electronically submit health claims
- Psychologists
Even cash-based providers who don’t submit claims are subject to the minimum use requirement of HIPAA, which means they must safeguard the privacy of patient records.
Next, take a look at your practices. Develop compliant processes to protect records, document security, and maintain the standards as your systems expand to accommodate an increase in employees and patients. According to the minimum necessary standard, an organization’s responsibilities come into play wherever health information is transferred. Therefore, you must dig into each instance where records change hands, including email, USB drives, and forms.
Areas to address to meet the HIPAA minimum necessary standard
Entities that deal with PHI look at the following areas:
- Disclosures from health providers about the treatment of a patient.
- Disclosures to patients about their records.
- Legally required disclosures.
- Disclosures within an organization across job roles.
- Disclosures to third-party business associates.
- Cybersecurity for PHI, computers, and data storage.
When Does the HIPAA Minimum Necessary Standard Apply?
The HIPAA minimum necessary standard applies to all covered entities that manage electronic health records (EHR) and documents, including the following examples:
- Spreadsheets
- Patient notes
- Diagnoses
- Identifying information, like birthdates and addresses
So, what is the minimum necessary use of an EHR? It’s the least amount of data required. But the minimum necessary standard regarding PHI includes broad access. It applies to spoken and printed records. It also applies to data stored in data centers and the cloud, or on computers and portable drives.
Third-party business associates who contract with covered entities must have a business associate agreement that requires them to comply with what doctors need to know for HIPAA compliance. These service providers can include medical transcriptionists, claims processing administrators, or cloud service providers (CSPs).
Besides the HIPAA minimum necessary rule, business associates must heed the HIPAA security rule to carry out duties that help keep data private. For example, if CSPs access PHI in their work, they need a contract that outlines their role in storing, destroying, and backing up data. They must agree on how to return records after their contract ends. Even if a CSP can’t decrypt medical data, they still meet the definition of a business associate when they receive electronic PHI (ePHI) records. These CSPs require a policy of disclosing the minimum necessary ePHI addresses and an established structure to report breaches.
What Are the Exceptions to the HIPAA Minimum Necessary Standard?
The HIPAA minimum necessary standard has the following exceptions:
-
- Disclosure required by law: This exception can include investigations by government agencies, like Child Protective Services, or follow-ups on workman’s compensation for an injury.
- Disclosure authorized by the patient per the HIPAA privacy rule: Patients can approve third-party use of their records, such as for research. They can also authorize disclosures with the opportunity to agree or object. For example, family members can informally pick up prescriptions on behalf of patients. Providers can notify family members of a patient’s location or condition with the patient’s informal permission.
- Public interest disclosure: Some disclosures happen for the public interest, such as the following examples:
- Providing information to the next of kin.
- Identifying a body.
- Transferring records to a medical examiner.
- Monitoring public health emergencies.
- Surveilling the healthcare system’s licensing.
- Disclosure of patient records: Covered entities can share medical records with the patient.
- Healthcare operations disclosure: This minimum necessary disclosure refers to records that support treatment, payment, and healthcare activities. They include:
- Care coordination.
- Fulfilling the required responsibilities for benefits coverage.
- Operations like quality assessment and case management.
- Incidental disclosure: Overhearing physicians in a hospital hallway is challenging to eliminate. If covered entities take reasonable steps to protect their patients’ privacy, it’s not considered a breach of the minimum necessary standard.
- Disclosure required by law: This exception can include investigations by government agencies, like Child Protective Services, or follow-ups on workman’s compensation for an injury.
What Are ‘Reasonable Efforts’ and ‘Reasonable Reliance’?
Reasonable efforts include any activities that a covered entity takes to protect patient privacy. They typically involve the following actions:
- Training workers on HIPAA “need-to-know” rule violations.
- Enhancing cybersecurity and tightening network permissions.
- Restricting access to data by job function.
- Encrypting transmissions.
Reasonable reliance is the standard that covered entities use when assessing requests for PHI. For example, a provider might reasonably rely on an insurance carrier to request the private health records or documents they need for the stated or intended purpose. They can interpret others’ statements as reasonably truthful if the records they request satisfy the inquiry. Covered entities must determine which parts of records are the minimum necessary to accomplish the task.
How to Comply with the HIPAA Minimum Necessary Standard
Complying with the HIPAA minimum necessary standard starts with understanding the types of PHI you need to secure. You might work with physical, telehealth, electronic, insurance claims, films, images, spoken health information, or all of these records. Regardless, you want a policy that defines the “reasonable efforts” you make to protect each one. Start with setting your standards and procedures.
Policies and procedures
- Have a written policy that defines the HIPAA minimum necessary standard for your organization. Consider the exceptions you need to make and to whom they apply. Also, think about what is minimally required to accomplish various tasks.
- Train employees on your policies. Make sure they know what information can be transferred, to whom, and under which circumstances. They should know what to do to enforce the HIPAA minimum necessary standard.
- Make a plan to monitor compliance. Know how easy it is to transfer just part of patient records upon request. Define which staff members need help implementing the policy. Establish a plan for onboarding new employees. Develop a system to carry out policies across departments.
- Document your compliance. Use logs and third-party software solutions to help monitor access and breaches.
- Talk about the importance of privacy. A compliance culture builds new employees’ buy-in and protects your workplace from HIPAA complaints. It also increases trust with patients.
The following principles and software tools help to automate security.
PHI discovery and classification
Use software solutions to detect sensitive data automatically, tag it across platforms, and mitigate the error-prone process of manually discovering and classifying sensitive data. By tagging fields, data teams can connect tags to HIPAA privacy standards to automatically handle them appropriately. Incoming data can also be classified automatically.
The Principle of Least Privilege
Limit access rights based on job roles with the Principle of Least Privilege (PoLP). This rationale aligns with the minimal necessary standard because it allows access at the most stringent level possible for executing job tasks. PoLP helps you restrict applications and processes.
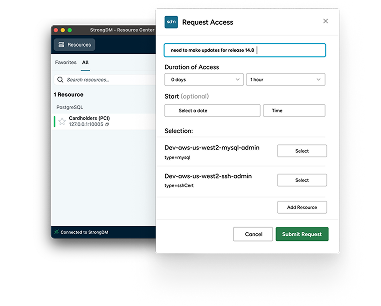
Just-in-time access
With the just-in-time (JIT) access security measure, you access records only within a designated time frame. This technology grants privileged, temporary access to protect records from malicious attacks. It also helps ensure that users who have permission get access to records only when they need them.
Monitoring access to PHI
Monitoring software links human resources data to medical records and creates activity reports to show who accessed and used the PHI data. It raises red flags about unusual access patterns so management can follow up to ensure the access is legitimate.
Implementing the Minimum Necessary Standard
The minimum necessary standard doesn’t have specific rules about what constitutes “reasonable effort” to protect patient privacy. Instead, let the specifics of your workplace guide you. Think about the kinds of records you keep, how and where you share them, and the physical and electronic safeguards you can implement to protect them.
More specifically, consider the following critical points:
- Know the categories and tags your existing data records contain.
- Develop comprehensive descriptions and standard operating procedures for job roles in your organization.
- Understand which data employees currently access to perform these roles.
- Train employees on the minimum necessary standard as it applies to your office and their roles.
- Create a mechanism for enforcing compliance.
- Plan the cybersecurity infrastructure needed to log and monitor your systems.
- Set up a system that generates reports and alerts in case of security breaches. Know who’s responsible for responding and if they follow a process.
- Be prepared to investigate any reported minimum necessary standard violation. Follow an established process.
Each point leads you toward establishing the core policies that build your own reasonable measures. Designing these policies, training employees, and designating a privacy officer to monitor and enforce them is the starting point for meeting the standard.
How StrongDM Helps With the HIPAA Minimum Necessary Standard
Safeguarding ePHI access frazzles even seasoned administrators, as healthcare organizations face unprecedented attacks. Patient records affected each year number in the hundreds of thousands. To protect patient privacy, minimizing access to records is crucial.
Ensure access for those who need it, exactly when they need it, to help secure your data with the StrongDM infrastructure access platform. From simple offboarding when employees leave to just-in-time access, StrongDM helps you manage privileged access, so tasks get done with fewer security risks. The StrongDM platform supports one of the most challenging parts of securing PHI—safeguarding access to electronic records—with less administrative work and better compliance.
Control access to your sensitive data, PHI, and EHRs, and meet the HIPAA minimum necessary standard. Try StrongDM free for 14 days.
Next Steps
StrongDM unifies access management across databases, servers, clusters, and more—for IT, security, and DevOps teams.
- Learn how StrongDM works
- Book a personalized demo
- Start your free StrongDM trial
Categories:

About the Author
John Martinez, Technical Evangelist, has had a long 30+ year career in systems engineering and architecture, but has spent the last 13+ years working on the Cloud, and specifically, Cloud Security. He's currently the Technical Evangelist at StrongDM, taking the message of Zero Trust Privileged Access Management (PAM) to the world. As a practitioner, he architected and created cloud automation, DevOps, and security and compliance solutions at Netflix and Adobe. He worked closely with customers at Evident.io, where he was telling the world about how cloud security should be done at conferences, meetups and customer sessions. Before coming to StrongDM, he lead an innovations and solutions team at Palo Alto Networks, working across many of the company's security products.
You May Also Like